ABSTRACT
Most of India’s people, and most of its poor,
still live in rural India. The burden of disease and its effects are disproportionately seen in the poor, with a clear ingredient in illness and mortality. There is a crisis in rural heath scenario in India and Bihar. There is widely prevalent myth that people in rural areas have small health problems which can be addressed by a minimally staffed and equipped heath centre. This paper completely debunks this illusion. People have a bewildering diversity of problems from HIV disease, advanced tuberculosis to severe malaria, uncontrolled diabetes with a low body weight and a badly infected wound to cancer of the cervix, a B.P. of 240/140 diagnosed for the first time in life. Delayed healthcare seeking because of difficulties of physical access, dissatisfaction with non-functioning or poorly functioning public health facilities, irrational care by an unqualified practitioner have further compounded the rural health scenario. This paper analyzes how rural people appreciate, complain and experience health, environment and their hygiene. The most disturbing and alarming observation is the Casteism factor impacting the government’s rural health programs in Bihar. The study was carried out in villages of remote border district of Madhubani in Bihar with prime objectives to assess and observe the heath status and family history of the people by Survey research method. Information and data were collected by personal interview during random visits to the village with the assistance and guidance of a qualified medical practitioner.
Key words: Rural Health, NRHM, Health Seeking Behaviour, Environment, Lifestyle, Casteism.
INTRODUCTION :
India is the second most populous country of the world and has changing socio-political demographic and morbidity patterns that have been drawing global attention in recent years. Despite several growth orientated policies adopted by the government, the widening economic, regional and gender disparities are posing challenges for the health sector. About 94% of health infrastructure, medical man power and other health resources are concentrated in urban areas where 73% of the populations live. Contagious, infectious and waterborne diseases such as diarrhea, amoebiasis, typhoid infectious hepatitis, worm infestations, measles, malaria, tuberculosis, whooping cough, respiratory infections, pneumonia and reproductive tract infections dominate the morbidity pattern, especially in rural areas. However, non-communicable diseases such as cancer, blindness, mental illness, hypertension, diabetes, HIV/AIDS, accidents and injuries are also on the rise. The health status of Indians, is still a cause for grave concern, especially that of the rural population. This is reflected in the life expectancy (63 years), infant mortality rate (51/1000 live births), maternal mortality rate (212/100 000 live births); however, over a period of time some progress has been made (Patil, 2012). To improve the prevailing situation, the problem of rural health is to be addressed both at macro (national and state) and micro (district and regional) levels. India continues to be dominantly agriculture dependent. India was the first country to launch family planning programme, and Malaria control programme had begun way back in 1953. We have flagship schemes such as that of NRHM and Janani Shishu Suraksha Yojana; still the situation in rural areas isn’t all motivating. This is all evident through some vital health parameters including increasing infant mortality rate, maternal mortality rate, poor state of sanitation, and prevalence of chronic diseases, non availability of qualified doctors and paramedical staff and so forth. These are particularly lagging behind in comparison to the situation in urban areas. Many of the villages still don’t have proper infrastructure for sub- centers and PHCs or CHCs. Even if they are there, they face unavailability of doctors or the staff, beds, basic medical equipments, drinking water supply and sanitation; any or at times all of them are in scanty numbers. The recent UP, NRHM scam unveils the serious irregularities in the ‘prime policies’ of the government at all levels from ministerial to executive. No concerted efforts have yet been made to raise the standards of sub-centers. There’s lack of diagnostic centers in villages; due to which patients, especially the serious one have to be carried along long distances that results in their deteriorating condition or even death. Moreover, ‘bad roads’ impede the movement of ambulances r any vehicle during emergencies. Inconvenient transport system is also a major concern. Shortage of funds is a major drawback in public health system (Mahobe, 2012 )
Bihar, the third most populous State in India, has recorded the highest population growth during the nineties. Recent times have also seen record GDP growth of 11.03 per cent over five years. Despite impressive economic growth, the benefits have not reached the poor, most of all children. Many disparities and inequalities persist, for example around 34% of Bihar’s population lives below poverty line. The major health indicators such as infant and maternal mortality are also much higher than the all India level, reflecting the poor status of child health in the State. Despite a modest decline in mortality figures over the past decade, the fact remains that 1 in 11.4 children still die within the first year of life, and 1 in 12 die before reaching age five. Bihar has one of the highest rates of infant mortality (29 per 1,000 live births) compared to just 7 in Goa and Kerala. The under-five mortality rate for Bihar is 56.4 deaths per 1,000 live births compared to the all India average of 35.73. The most recent National Family Health Survey (NFHS-5, 2005-06) indicates some improvement in immunization coverage, contraceptive use and institutional deliveries. However, malnutrition among children and women has actually increased in recent years. Malnutrition among children has increased from 41% to 44%, while the number of children showing wasting (weight for age) has gone up by 2%. Anaemia has gone up from 31% to 37% amongst children of 6-59 months. Health researchers have paid little attention to the role of place in health except as settings where interventions take place and even less attention have been given to the influence of rural context on health (Thurston, 2003). Health is not merely an issue of doctors, social services and hospitals, but also an issue of social justice is involved. Among the definitions are still used, probably the oldest is that health is the absence of disease. In rural areas people have many problem related to health (Park and Park, 1989). Healthcare continues to be a neglected aspect, however, during the past few decades; there has been a reawakening to establish that health is a fundamental human right and, that it is essential to the satisfaction of basic human needs.
There are two ways in which the environment affects human health. First is directly through pollutants discharged by industries into the air and water by automobiles. Human health is also affected by the quality of environment at the place of work (Eve et al, 2007). The deterioration of environment such as existence of stagnant water pools in villages provides fertile ground for breeding of vectors. Malaria which was once thought to have been eradicated, has reached endemic proportions in many parts of country (Kruger et al, 2001).
Study Area :
The present study was carried out in four villages of Madhubani district with main objective being to assess the health status and family history of the people residing in the village. Health related problems amongst the villagers are quite acute. These problems are due to their erratic life style, poor sanitation and bad environmental condition prevailing in the village The district of Madhubani was carved out of the old Darbhanga district in the year 1972 as a result of reorganization of the districts in the State of Bihar. This was formerly the northern subdivision of Darbhanga district. It consists of 21 Development Blocks. Bounded on the north by a hill region of Nepal and extending to the border of its parent district Darbhanga in the south, Sitamarhi in the west and Supaul in the east, Madhubani fairly represent the centre of the territory once known as Mithila and the district has maintained a distinct individuality of its own. It is located at a Longitude of 25º- 59' to 26º-39' east and the Latitude is 85º-43' to 86º-42' north. The Madhubani district is situated at height of 80 meters from Sea. Madhubani occupies a total of 3501 sq. kms. High Flood Level is 54.017 m. Whole District is under Earthquake Zone 5. Rainfall varies between 900 mm and 1300 mm. Average Rainfall = 1273.2 mm. The climate of the region may be described as composite with hot and dry summers, hot and humid rainy season and short autumns and winters. Mean maximum temperature in summers is 33°C, with the highest maximum of 41°C and mean minimum temperature in winters is 18.5°C with the minimum range of 3-4°C (Govt. of Bihar, 2012). The sampling sites for the study were Jonki, Chhatauni, Mahinathpur and Simrarhi villages of Madhubani District of Bihar. These sites were selected based on random sampling technique.
METHODOLOGY :
The present study was carried out in different villages of Madhubani district of State Bihar, with main objective being to assess and observe the health status and family history of the people inhabiting the villages in Madhubani. In the present survey research administered survey or interviews were used to collect and gather information from the respondents. Information and Data regarding various parameters, including health diseases, gender, educational status, annual income, addiction, immunization, and family planning were collected by personal interview with the respondents in their homes during random visits to the village. Blood groups were determined by antiserum method with the assistance of trained technician from the local private pathological lab at Jayanagar, Madhubani. Blood pressures were measured by the oscillatory method with the help of Stethoscope and Sphygmomanometer. Altogether, 27, 25, 23, 24 families and a total of 125 males, 96 females; 92 males ,69 females ; 119 males, 100 females and 99 males and 77 females were selected randomly from Jonki, Simrarhi, Mahinathpur and Chhatauni respectively his constitutes 10% of the sample and information was collected by personal interview in their homes. 300 people were selected randomly from the total population belonging to different age groups and they were observed personally and interviewed, tested and measurable data by various tests and instruments respectively.
Situational Analysis :
It was clear that, villagers did not see rurality overall as a threat to their health. Defined the reputation of a neighbourhood as ‘how areas are perceived by their residents, outsiders and service or amenity planners and providers (Macintyre, 2000). If health promotion practitioners characterize rural areas as ‘high risk’, focus on the occupational health threats of farming, or otherwise suggest that their view of an area is negative, this may be at odds with the views held by residents and create communication problems. Moreover, people who were interviewed relate most of the problems to the background pollution that is emanating from the nearby brick chimneys. Diabetes is a serious health problem in these villages. The scientific evidence is clear: that diabetes in these villages is largely a result of an introduced diet and shifting lifestyle. Poverty and remoteness of communities on the reservation contribute to the problem. Proper exercise or shifting towards their earlier village lifestyles viz producing fruits and vegetables, closer to home in an individual or community setting, fetching water from local rivers, caring for animals etc will reduce the burden. Gardening is a component of diabetes care but a multi-sectored approach involving agriculture, nutrition, health, \policy-makers, community leaders, schools and individuals is required to make faster progress on curbing diabetes in the these villages (Lombard et al, 2006). Skin diseases are common among rural people worldwide and most of the researchers have correlated this disorder to underlying socio-demographic and hygiene factors. It is therefore recommended that regular skin examination is performed in rural areas in order to identify people with skin disorders and to help them to understand the importance of effective personal hygiene. It is often stated that overcrowding and poor living conditions favour the development of many skin diseases (Dogra and Kumar, 2003).
Tobacco use leads most commonly to diseases affecting the heart and lungs, with smoking being a major risk factor for heart attacks, strokes, chronic obstructive pulmonary disease [COPD] [Including emphysema and chronic bronchitis] and cancer [particularly lung cancer, cancers of the larynx and mouth and pancreatic cancer. It also causes peripheral vascular disease and hypertension among the rural population (Vainio, 1987). The rural population in Bihar faces immediate health consequences, such as more shortness of breath, poorer levels of fitness and increased phlegm production. Targeting teens is particularly important because only 10% of adult smokers start after the age of 18 years. Our findings suggest that the anti-tobacco actions that have decreased tobacco use nationally should incorporate strategies aimed at addressing tobacco use in rural settings. Because the rate of smokeless tobacco use was also found to be higher in rural areas, customizing anti-tobacco campaigns for rural youths to address the use of smokeless tobacco products may result in a larger decrease in the overall smoking rate in this population. It has been found, that urinary tract infections occur more commonly in women than men in the rural settings. Pyelonephritis usually follows a bladder infection but may also occur from a blood borne infection and lack of hygienic conditions among rural areas of Bihar. Urinary tract infections are the most common cause of hospital acquired infections in rural as well as in urban areas, accounting for approximately 40%. The rates of asymptomatic bacteria in the urine increase with age from two to seven percent in women of child bearing age to as high as 50% in elderly women in care homes (Brunner, 2010).
It is important to note that in the Northern India healthcare system, patients may contact a specialist without a referral from the primary care physician and severe cases could be lost. In rural areas of Bihar, patients who are experiencing only minor symptoms are more likely to consult the local non- specialized physician, who visits their village, instead of travelling to healthcare centers or to distant urban specialized doctors. The possible explanations for the high rates of acidity may be found in the socio-cultural environment and the northern Indian diet. The primary aim of decentralization is to increase the resource base for primary care, by shifting as many resources as possible from central to peripheral locations. A second aim is expand the ‘decision making space’ of middle and lower level managers, in order to increase the responsiveness of sub national authorities to local health needs and situations.
Table 1. Sex wise age groups of the study population in selected villages
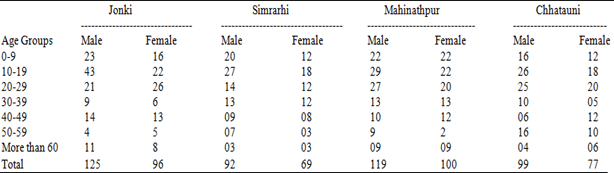
Table 2. Sex wise education status [%] of the study population
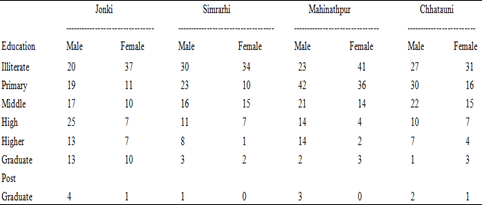
The data is expressed as the percentage to the nearest figure
Table 3. Sex wise addiction in the study population
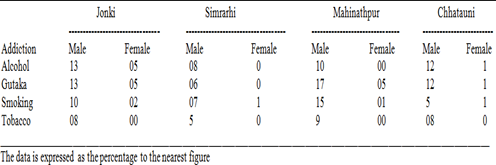
Table 4. Sex wise average blood pressure in the study population
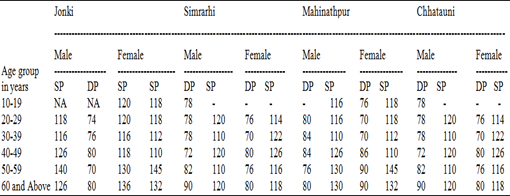
Table 5. Sex wise prevalence of different diseases/ symptoms in the study population
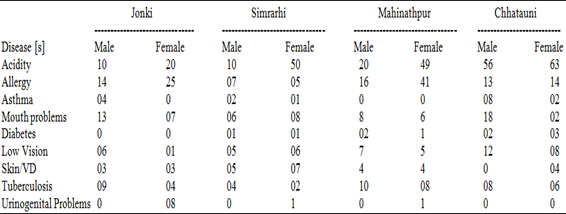
The data is expressed as the percentage to the nearest figure
It has been found that one of the most extensive levels of decision-making in an administrative sense (Bossert, 2002). In reality, however, there is evidence to suggest that decision- making often can be constrained in the devolved context by political priority setting of local authorities, which can sometimes be perceived by health managers to be in conflict with priority setting based on health needs. A third aim of decentralization is to enhance. The efficiency and effectiveness of health services management through prompt and appropriate middle level management decision-making. This is consistent with some been associated with the complication of efforts to construct a logical hierarchy of health services, mainly due to the existence of ‘grey areas’ of responsibility between system levels and the lack of preparation of middle level management to take on new roles (Mills et al, 1990). A family support is also important in raising the health conditions of rural people as there is strong association between family support and health status of people (Shoaib Muhammad et al, 2011).
Caste Affecting Rural Health Plans in Bihar :
In what could be perceived as a disturbing trend, vaccination in rural Bihar has been adversely affected due to Casteism .According to the recent survey report, which was prepared after an on-the-spot study in 14 villages of Bihar’s nine districts, several instances of “caste discrimination” have came to fore. For instance, such was the social divide in a Rohtas village that vaccinations could not take place either in Brahmin’s tola (colony) or Paswan’s tola simply because the Brahmins refused to go to the Paswan tola, or allowed them to enter their area. All this, when the vaccination had to take place at the anganwadi centre (Deccan Herald, 2012).
Equally disturbing was the trend at Chhatauni village in the Madhubani district where Paswan children were summoned only when there was an inspection, although the head count was regularly maintained. Similarly, the caste of “Asha workers” (Accredited Social Health Activist) too played a role in non-inclusion of poorer groups in the social welfare programmes. While, the Asha workers are key functionaries and integral part of the rural health system related to deprived sections of the society, it was found in the study that they received cooperation (or no cooperation) depending on their own caste. Surprisingly, in the Chhatauni village, upper caste Rajput and Yadav women had no inhibitions in admitting that they did not cooperate with the Asha workers because they belonged to lower castes.
Notably, it’s the Asha workers who, of late, have replaced village mid-wives and play a crucial role in child delivery. The report, prepared by the Institute for Development Research (IDR), however, has something positive to suggest. Villagers now look for institutional deliveries and believe that hospitals are much safer place to give birth. Under the Centre’s ambitious scheme - “Janani Suraksha Yojana”, institutional deliveries have escalated from 8, 38,481 in 2016-178 to 11, 43,039 in 2018-19. The saving grace, as per the report, is that there is no caste discrimination at the primary health centers (PHCs) (Ibid).
Conclusion :
The conducted survey created a new finding to form the basis of policy initiatives and a model of utilization of health services by the residents of the rural villages of Madhubani district. The rural communities struggle with maintaining healthcare services, supporting the rural health care safety net is critical. The mentioned factors are among the most significant barriers to equitable care and must be addressed in order to eliminate healthcare disparities, particularly among rural People. Through innovative strategies such as bringing health care to the community via a mobile medical clinic, inter-agency collaboration, involvement of students in the program and utilization of programs for information, referrals, support and lay education will make a positive impact on rural people of Bihar. Women especially in the village need to be empowered in areas of income generation, education and their role in social upliftment to enable them access to health services. Health facilities must be equally distributed to ensure equal physical access. Rural development needs focus on methods that lead directly to sustainable programmes to promote the health of rural community. Improving rural health requires innovative, creative and integrative strategies that address both individual health related behaviours and many social determinants of health. It is imperative for any planning effort to think beyond health care services to the more multifaceted social conditions that impact health. We do have the schemes, policies and programmes in our hand, but even after repeatedly being brought into notice and concern, the implementation has been pitiful. It’s much hoped and needed that a proper feedback mechanism and audit be instituted and timely watched with a ‘political will’ in place. So that then rural India that constitutes around 70% of population is not ailing but smiling.
REFERENCES :
- 1. Bechelli, L.M., N. Haddad and W.P. Pimenta, 1981, “Epidemiological survey of skin diseases in school children living in the Purus Valley [Acre State, Amazonia, Brazil]”. Dermatologica, 163: 78-93.
- 2. Bossert, T. and J. Beauvais, 2002, “Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space”. Health Policy and Planning, 17: 14-31.
- 3. Brunner and Suddarth's, 2010, Textbook of medical-surgical nursing. [12th Ed.]. Williams and Wilkins, Philadelphia: 1359.
- 4. Collins, C. and A. Green, 1994, “Decentralization and primary health care: some negative implications in developing countries”. International Journal of Health Services, 24: 459- 475.
-
5. Deccan Herald, 29 April, 2012
- 6. Dielubanza, E.J. and A.J. Schaeffer, 2011, “Urinary tract infections in women”. The Medical clinics of North America, 95(1): 27-41.
- 7. Dogra, S. and B. Kumar, 2003, “Epidemiology of Skin Diseases in School Children: A Study from Northern India”. Pediatric Dermatology, 20: 470-473.
- 8. Eve, W., J. Manisha, T.A. Kristie and A.M. Laura, 2007, “Measuring the effect of intimate partner violence on health-related quality of life: A qualitative focus group study”. Health Quality Life Outcomes, 5: 67 doi: 10.1186/1477-7525-5-67
- 9. Figueroa, J.I., T. Hawranek, A. Abraha and R.J. Hay, 1997, “Prevalence of skin diseases in school children in rural and urban communities in the Illubabor province, south- western Ethiopia: a preliminary survey”. Journal of the European Academy of Dermatology and Venereology, 9: 142-148.
- 10. Govt. of Bihar, 2012, Madhubani District Health action plan, State Health Society Patna Harris, M., D. Nako, T. Hopkins,
D.M. Powell, C. Kenny, C. Carroll, et al. (1989) “Skin infectionsin Tanna, Vanuatu in. Papua New Guinea” Medical Journal, 35: 137-143.
- 11. Kruger, A., A. Rech, X.Z. Su and E. Tannich, 2001, “Two cases of autochthonous Plasmodium falciparummalaria in Germany with evidence for local transmission by indigenous Anopheles plumbeus” Trop. Med. Int. Health, 6: 983-985. Doi: 10.1046/j.1365-3156.2001.00816.x
-
12. Lombard, K.A. S. Forster-Cox, D. Smeal and M.K. O'Neill, 2006, “Diabetes on the Navajo nation: what role can gardening and agriculture extension play to reduce it?” Rural and Remote Health 6: 640. [Online] Available: http://www.rrh.org.au
-
13. Macintyre, S, 2000. “The social patterning of exercise behaviours: the role of personal and local resources”. British Journal of Sports Medicine, 34: 1-6.
-
14. Mahobe, R, http://www.youthkiawaaz.com/2012/09/rural- health-scenario-in-need-of particular-attention/
- 15. Mills, A., P. Vaughan, D. Smith and I. Tabibzaquedeh, 1990, Health System Decentralization. Geneva: WHO.
- 16. Park, J.E. and K. Park, 1989, Textbook of Preventive and Social Medicine. 12 h, Jabalpur. Bhanot Publishers.
-
17. Patil, A.V et.al, 2012, “Current Health Scenario in Rural India”,
Aust. J. Rural Health, 10, 129-35
- 18. Thurston, W.E. and L.M Meadows, 2003. “Rurality and health: perspectives of mid-life women.” Rural and Remote Health 3: 219. [Online]. Available: http://www.rrh.org.au.
- 19. Vainio, H, 1987. “Is passive smoking increasing cancer risk?” Scand J. Work Environ Health, 13(3): 193-196.